Men and women use a variety of contraceptives to prevent pregnancy. Most of these methods are temporary and reversible. But some people resort to radical contraception. These are a tubal ligation for females and a vasectomy(male sterilization) for male persons. Below we will tell you about the basic facts that you need to know about vasectomy.
Some Historical Facts
The first vasectomy surgery was done on a dog in 1823. A short time after that, British doctor R. Harrison performed an operation on a man not for the purpose of contraception, but to cause atrophy of the prostate. At the beginning of the 19 century, American surgeons used vasectomy in penitentiary facilities with the intention to prevent the birth of future criminals. Apparently, this practice was associated with Cesare Lombroso’s theory of anthropological criminology (the concept of a ?born criminal?), which was popular at that time.
Vasectomy began to be used as a method of birth control during World War II (about WWII). For the first time, a national-level vasectomy program was introduced in 1954 in India. Now vasectomy is available in many countries worldwide.
Vasectomy ? Definition and Legal Issues
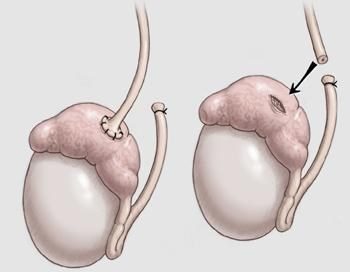 Vasectomy is a surgical operation, during which the removal, bandaging or clogging of a fragment of the vas deferens in males is carried out. The procedure results in sterility (i.e., inability to have offspring), but sexual functions are preserved. Vasectomy has no effect on male libido, erection or the possibility of ejaculation. The appearance of sperm remains normal. Men who have undergone the surgery do not appear to be at increased risk for testicular and prostate cancer.
Vasectomy is a surgical operation, during which the removal, bandaging or clogging of a fragment of the vas deferens in males is carried out. The procedure results in sterility (i.e., inability to have offspring), but sexual functions are preserved. Vasectomy has no effect on male libido, erection or the possibility of ejaculation. The appearance of sperm remains normal. Men who have undergone the surgery do not appear to be at increased risk for testicular and prostate cancer.
Related Topic: Prostate Cancer and its Risk Factors
In Canada, there are no laws that prohibit voluntary sterilization (tubal ligation in females or vasectomy in men). The spouse’s consent isn’t required by laws.
However, the doctor may require that the husband obtain the consent of his wife for the operation. Additionally, he / she may refuse to perform the surgery if a couple is very young and doesn’t have children.
In the United States, before performing vasectomy, a patient should provide a written consent containing the following points:
-
that he requests an operation to prevent paternity in the future;
-
that he understands that the operation may not cause sterility;
-
that he agrees to submit sperm samples for analysis and use contraception until the analysis shows that he is sterile.
Effectiveness of Vasectomy
Vasectomy is a highly efficient (around 99.8%) birth control option. According to the study by J. Trussell et al. (2011), only 1?2 females out of 1000 had unplanned pregnancy during the 1st year after their males had had vas deferens surgery.
Nevertheless, the operation is associated with minor risk of failure.
Pregnancy is possible after a sexual intercourse with a man who has undergone vasectomy due to:
-
not using another birth control option until spermatozoa in sperm are confirmed to be absent (typically this result is achieved after 10?20 ejaculations, which allow to completely remove spermatozoa from male organs);
-
unprompted re-joining of vas deferens or a small opening resulting in mixing spermatozoa with sperm (such situations are very rare).
How is Vasectomy Performed?
Before the procedure, the testicles and scrotum of the patient are cleaned with an antiseptic. Hair can also be shaved. Vasectomy does not require general anesthesia and is performed under local anesthesia.
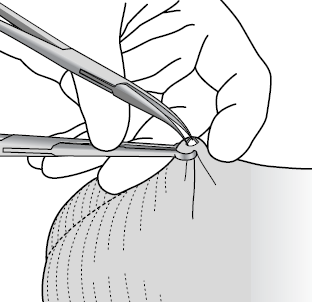 The two typical surgical approaches for providing access to vas deferens during the procedure are the traditional incisional option and no-scalpel (NSV) technique. The ordinary incisional technique is carried out with the help of scalpel to perform 1?2 incisions. If NSV technique is applied, the surgeon uses sharp instrument looking like a forceps in order to puncture the skin. This approach is developed to reduce the risk of adverse events, such as pain, infection on the puncture site, and bleeding.
The two typical surgical approaches for providing access to vas deferens during the procedure are the traditional incisional option and no-scalpel (NSV) technique. The ordinary incisional technique is carried out with the help of scalpel to perform 1?2 incisions. If NSV technique is applied, the surgeon uses sharp instrument looking like a forceps in order to puncture the skin. This approach is developed to reduce the risk of adverse events, such as pain, infection on the puncture site, and bleeding.
Through the incisions, the surgeon cuts the vas deferens. The ends of the ducts are sutured, bandaged or clogged. For this purpose, the electrocoagulation technique can be applied. Scar tissue, formed after a vasectomy, helps to block the ducts.
Another technique for performing the intervention is implanting the Vasclip clip. It involves blocking the duct with an implant. It is believed that the introduction of implants reduces the risk of chronic pain after the operation. However, a study by D. Kirby and others (2006) showed that the incidence of adverse events after Vasclip implantation was the same as after applying standard techniques. However, patients who participated in this study found the procedure with Vasclip more preferable than conventional vasectomy.
Pros and Cons of the Procedure
The operation has both advantages and disadvantages. Let’s take a closer look on them.
Pros
- Better sexual intercourse. The procedure can positively affect the intimate relationships of partners because they now do not have to worry about unwanted pregnancies.
- Great effectiveness. As we have mentioned above, the effectiveness of the procedure is about 100%. It is an ideal option for couples who do not want children in the future.
- It is a safe & minor operation. Vasectomy is characterized by high safety profile. Complications (like bleeding, infections, inflammatory processes, and so on) are very rare, but they may occur. Vasectomy doesn’t require long time to recover. A male will return to normal life 1 week after the surgery.
Cons
- Some males get depressed after it. Some patients reported a worsening of mood after vasectomy due to the realization that they would not be able to reproduce.
- Difficult reversibility. The only way to restore the ability to have offspring after the procedure is the so-called reverse vasectomy (or vasectomy reversal), which involves the re-joining of the vas deferens. Reverse surgery is a very costly and technically difficult technique, which may not yield the desired result, especially if much time has passed after sterilization.
- Possible pain. Some male persons suffer from chronic pain in the testicles which appears immediately or a few months after the surgery.
- It doesn’t protect from STDs. A couple still need to use condom in order to prevent sexually transmitted diseases including HIV.
Conclusion
If you’re considering to see a doctor to make vasectomy, you should be 100% sure that you will not want a child in the future. The surgery may be reversible, but it costs money. Additionally, there is no guarantee, that vasectomy reversal will be successful. So, make an informed and well-considered decision.





